Deep Learning vs Traditional Breast Cancer Risk Models to Support Risk-Based Mammography Screening
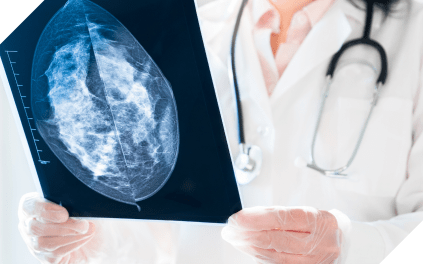
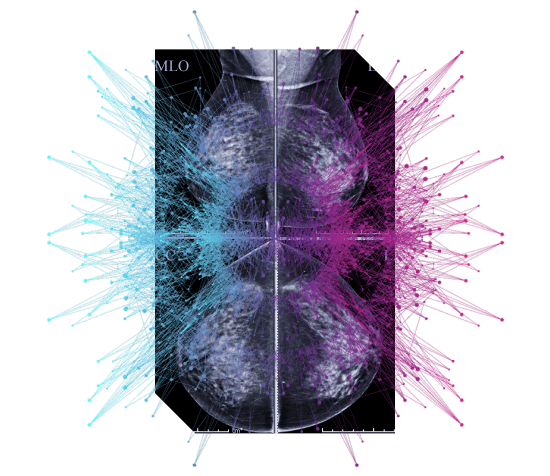
Deep learning breast cancer risk models demonstrate improved accuracy compared to traditional risk models. This research highlights the promise deep learning models to support equitable, risk-based mammography screening.